Didier Torny, Sociologist, Centre de sociologie de l’innovation, (Mines ParisTech, CNRS)
Frédéric Vagneron, Historian, Centre Alexandre-Koyré (EHESS, CNRS, MNHN)
Never has the genetic identification of a new virus been deciphered so quickly: on the 29th of December 2019, the first cases of an epidemic caused by a new virus are reported in China; 7 days later, a team from Fudan University in Shanghai publishes the complete sequence of the RNA virus of the coronavirus family. Since then, the sequences of its variants have been accumulating on the website nextstrain.org with more than 120 identifications by teams from 20 countries.
Widely reported in the media, the accelerated discovery points to a little known facet of social networks, their intensive collaborative use by scientific communities. It comes in the context of the open science revolution. While the results of the SARS epidemic in 2003 still required weeks, the hyper-speed of data exchange on the new SARS-CoV-2 coronavirus bypasses traditional channels of scientific communication. Preprints are now much more rapidly disseminated than scientific journals articles, and are setting the pace.
This acceleration in the production of knowledge presents risks, such as the limited assessment of results or the sharing of fragmentary, if not erroneous, data. But they are collectively assumed by the communities that otherwise organize the discussion among peers, going so far as withdrawing preprint deemed insufficient or misinterpreted within days.
A Story of Microbe Hunters
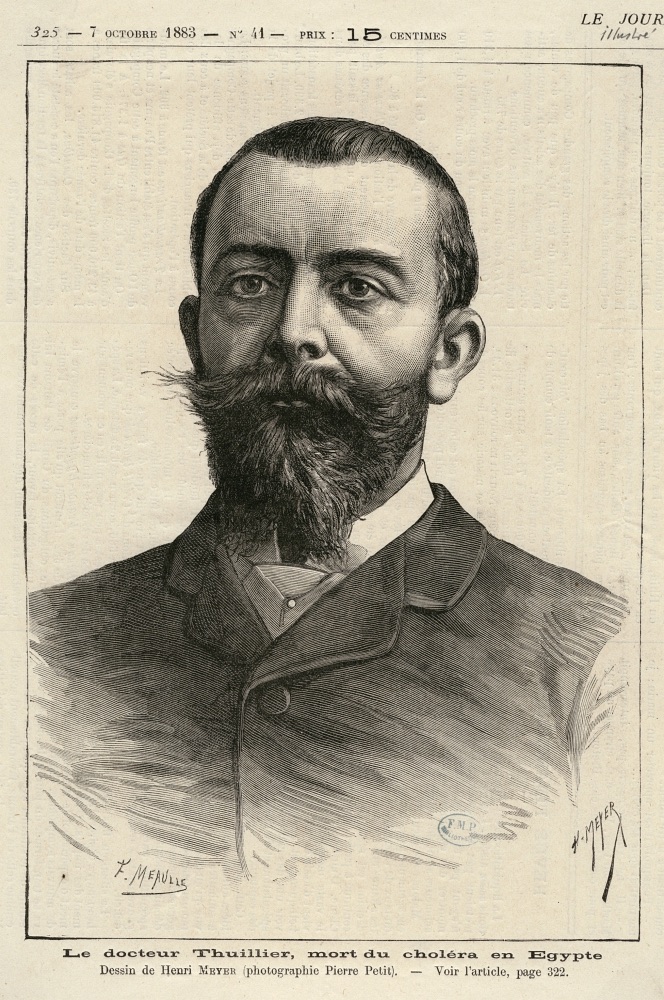
However, identifying a pathogenic microorganism, regardless of its virulence, is a difficult task. The history of “microbe hunters” is as old as bacteriology, which originated at the end of the 19th century. As early as 1883, Pasteur’s and Koch’s teams competed on the Egyptian ground to be the first to identify the cause of the cholera epidemic raging in the arena: a young French researcher, Louis Thuillier, died in the process and the German commission won the race. Widely reported in the new telegraphic press of the time, national interest and prestige prevailed. In 1890, faced with the flu epidemic that was sweeping through Europe, Louis Pasteur was cautious about the race to publish. Harassed by questions about which “microbe” was involved, he became annoyed: “I don’t know. Once again, what can one say without proof?” Before concluding: “We don’t know, I tell you, we have to look” (L’Echo de Paris).
The 20th century has seen an exponential development of knowledge about infinitely small living organisms. Virology, as soon as the 1930s, provided a remarkable quantity of new microorganisms for several decades. The coronavirus family was thus identified by British teams in the mid-1960s. It was at this time that genetic knowledge began to allow routine identification of microorganisms from biological samples. This multiplication of knowledge does not depend solely on the ingenuity of researchers: it requires infrastructures and standardised practices that allow the circulation of strains, the control of experimental results, and later clinical trials.
The role of scientific organisations, but also military organisations, has long been crucial in this sharing of knowledge such as in that of strains and reagents. But the interests are divergent: the so often mentioned international “solidarity” of researchers is a political construction. The World Health Organization (WHO), heir to the Hygiene Organization of the League of Nations, is a pioneer in establishing this cooperation between scientists. To act as an alarm raiser, the Geneva-based organisation developed a system of worldwide networks of laboratories specialising in the study of new pathogens. The Influenza Program, established in 1948, brings together international teams organized around the World Influenza Centre in London to monitor viruses with intriguing variability. However, collaboration doesn’t always meet all the expectations: during the AIDS pandemic, the identification of the retrovirus, which lasted several years, led to a scientific and financial battle between American and French teams.
International alerts due to a lack of sustainable resources
Since the 1980s, the WHO-dominated international public health, has undergone profound and lasting changes. Faced with budgetary constraints due to stagnating contributions from Member States, the challenges of an HIV pandemic to which it has been slow to respond, and the multiplication of private and public actors, WHO has refocused its activities on surveillance and alert. The development of primary care structures and access to essential medicines, initiated in the 1970s, has been downgraded behind new priorities, including the surveillance of emerging diseases. With H5N1 (1997, 2005), SARS (2003) and H1N1 (2009), investment in early warning and surveillance is proving to be an effective yet risky way of maintaining WHO’s prestige in the era of global health.
Mostly implemented by the wealthiest countries, the preparedness plans initiated by WHO since the 1990s aim to define the political, social, alimentary and sanitary ways of life in crisis situations and the interruption of the circulation of goods, medicines and protective devices. But they cannot compensate for the lack of sustainable investment in basic public health infrastructures, which alone can carry out prevention campaigns and build the confidence of populations in low-income countries. Last December, the WHO’s emergency unit (GOARN) issued a statement indicating that 140,000 people have died from measles in 2018, a disease for which preventive vaccines have been developed since the 1960s. In response to the Covid-19 outbreak, the WHO Director-General launched a US $675 million emergency aid package to aleviate – sad euphemism – «different levels of effectiveness in national preparedness and response measures”. The sum seems quite paltry.
As unprecedented as it may be for the scientific community, the rapid identification of the virus cannot make it possible to reduce global health inequalities and their consequences, which become more visible in times of crisis. Borders are not only temporarily closed to travelers from “at risk” areas, they define territories that are durably isolated from “global” solidarity.
Tribune published in Libération on March 5, 2020 , “Covid-19, les frontières se ferment et la science diffuse” [Covid-19, borders are closing and science is spreading]
Read more:
Torny Didier (2012). De la gestion des risques à la production de la sécurité. L’exemple de la préparation à la pandémie grippale, Réseaux, 171, 45- 66.
Vagneron, Frédéric (2015). Surveiller et s’unir : Le rôle de l’OMS dans les premières mobilisations internationales autour d’un réservoir animal de la grippe. Revue d’anthropologie des connaissances, 9, 2(2), 139-162. doi:10.3917/rac.027.0139.
Image 1 – Photo source: Prachatai, Covid-19, March 2020. Flickr. (CC BY-NC-ND 2.0)
Image 2 – Source: Dr Thuillier, mort du choléra en Egypte [Dr. Thuillier, who died of cholera in Egypt], Drawing by Henri Meyer (photography by Pierre Petit), Le journal illustré, 7 October, 1883. Collection BIU Santé Médecine, Université de Paris. (Open License)
Image 3 – Photo source: Duncan C., Coronarivus, 6 March, 2020, Flickr. (CC BY-NC 2.0)

